Meningococcal meningitis is a serious infection of the meninges (tissues covering the brain and spinal cord) and blood infection, which develops strongly in winter and spring...
1. What is meningococcal meningitis?
Meningococcal meningitis (MM) is a form of bacterial meningitis, a serious infection of the meninges, causing brain damage, with a mortality rate of about 50% if left untreated. The disease is caused by many types of bacteria, including Neisseria meningitidis (N.meningitidis). Up to 12 serogroups of N. meningitidis have been identified as the culprit, 6 of which (A, B, C, W, X and Y) can cause pandemics.
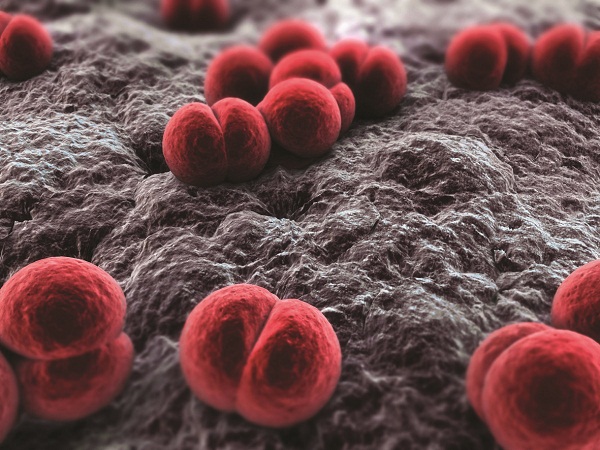
Neisseria meningitidis bacteria, the culprit that causes meningococcal meningitis
2. How is the disease transmitted?
Meningococcal bacteria are transmitted from person to person through respiratory droplets or from the throat released into the air. Close and prolonged contact such as kissing, sneezing or coughing on someone, or living near an infected person, sharing food, drinks, or household items with an infected person can easily spread the disease. The incubation period is on average 4 days, but can range from 2 to 10 days. N. meningitidis only infects humans; animals do not contain the pathogen. Scientists believe that 10% to 20% of the general population of the world carries N. meningitidis in their throats at any time in their lives. The rate of disease transmission may be higher during epidemics, harsh climates, or poor eating, hygiene, and disease prevention.
3. Symptoms
The most common symptoms of MN are stiff neck, high fever, sensitivity to light, confusion, headache, and vomiting. Even with early diagnosis and appropriate treatment, 5% to 10% of patients die, usually within 24 to 48 hours of symptom onset. Bacterial meningitis can cause brain damage, hearing loss, or learning disabilities in 10% to 20% of survivors. A rare but highly fatal form of MN is meningococcal septicaemia, characterized by a hemorrhagic rash and rapid circulatory collapse.

Meningococcal meningitis patient
4. Diagnosis
The initial diagnosis of meningococcal meningitis is made by clinical examination followed by a lumbar puncture, which reveals purulent spinal fluid. Bacteria may occasionally be found on microscopic examination of the cerebrospinal fluid. The diagnosis is supported or confirmed by culturing the bacteria from a sample of cerebrospinal fluid or blood, by agglutination testing, or by polymerase chain reaction (PCR). Serogroup identification and antimicrobial susceptibility testing are considered important for appropriate disease screening.
5. Treatment
Meningococcal meningitis is a potentially fatal disease and should be treated as a priority. Hospital admission is required as soon as possible, and isolation is not necessary. Appropriate antibiotic treatment should be started as soon as possible, especially after the lumbar puncture has been performed. If treatment is started before the lumbar puncture, it may be difficult to culture the bacteria in the cerebrospinal fluid for diagnosis. A range of antibiotics can be used to treat the infection, including penicillin, ampicillin, chloramphenicol and ceftriaxone. Ceftriaxone is preferred in some economically disadvantaged countries such as sub-Saharan Africa when there is an epidemic.

Vaccination is the best way to prevent meningococcal meningitis
6. Prevention
There are currently three types of vaccines to prevent meningococcal meningitis:
Polysaccharide vaccines, which have been available to prevent the disease for more than 30 years, are available for diphtheria serogroups A and C, triphtheria serogroups A, C, and W, or serogroups 4 (groups A, C, Y, and W).
For serogroup B, a polysaccharide vaccine could not be developed, due to antigenic similarity to polysaccharides in human nerve tissues. The first vaccine against NmB, made from a combination of four protein components, was officially introduced in 2014.
Since 1999, meningococcal conjugate vaccines against serotype C have been available and widely used. Tetravalent A, C, Y, and W conjugate vaccines have been licensed since 2005 for use in children and adults in the United States, Canada, and Europe.
7. Outbreak Trend
According to WHO, meningococcal meningitis occurs in small clusters on a global scale, fluctuating seasonally. The heaviest burden of meningococcal meningitis is currently in Sub-Saharan Africa, known as the meningitis belt, stretching from western Senegal to eastern Ethiopia. During the dry season from June, dusty winds, cold nights and respiratory infections damage the nasopharyngeal mucosa, increasing the risk of MN. Outbreaks of N. meningitidis are also due to poverty, overpopulation and poor hygiene, especially during the dry season. To limit the risk of disease spread, WHO recommends that countries strengthen prevention and response. Vaccination for people aged 1-29 with the MENA conjugate vaccine is considered the most optimal and effective solution today.
Dr. Chu Trang Nhung - Suckhoedoisong.vn

